The right health insurance plan protects you and your loved ones in case of illness or accident, ensuring that you can afford the medical care you need. There are many different types of health care plans available in the United States, and the options can be overwhelming. Understanding your options will help you select the provider model that best suits your needs. This guide lays out the most common types of health insurance plans.
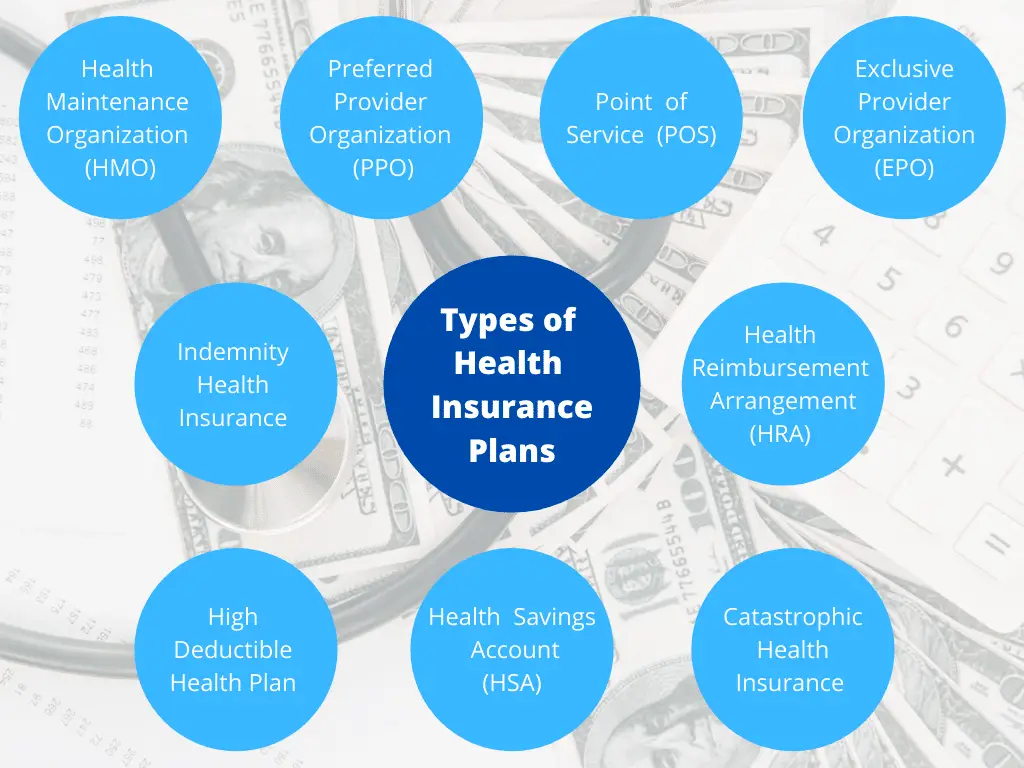
Health Maintenance Organization (HMO)
A health maintenance organization or HMO plan is among the least expensive coverage options. What’s the catch? You are limited to a select list of providers (doctors and hospitals) who have agreed to participate in the HMO. This list can be quite short.
If you have to see a specialist, you may need to get a referral from your doctor. Some HMOs also have a “closed network” model, meaning you won’t get any reimbursement if you see providers outside of the HMO.
Preferred Provider Organization (PPO)
Preferred Provider Organization or PPO health insurance gives you a bit more flexibility than the HMO insurance plan. When you enroll in a PPO, you receive a list of preferred providers. These are doctors and hospitals that have agreed to participate in the plan, referred to as network providers.
If you go to these providers, you will have to pay less than going to an out-of-network provider. In that case, you will have to likely pay a larger portion out of your own pocket. There are also Medicare PPO plans available.
Point of Service (POS)
A point-of-service plan is a managed-care insurance plan that basically combines the qualifies of an HMO and a PPO. You get different benefits depending on whether you use providers that are in or out of the network. Policyholders are required to choose a network primary care physician while on a POS plan. Primary care doctors can then provide referrals to specialists.
You will have to pay more medical costs yourself if you see providers outside of the plan’s network. The costs of POS plans tend to be lower. However, the list of health services providers may prove restrictive.
Exclusive Provider Organization (EPOs)
With these types of plans, policyholders are permitted to see doctors and hospitals within the specified EPO network — but can’t go beyond the network for care. You will not get any coverage for out of network health services.
You can negotiate a lower rate with an EPO than you would with an HMO or PPO. However, you risk having to pay for your own care, for example, if you see a specialist. An EPO may be the right option for you if you are comfortable with a limited selection of health care services providers in exchange for lower rates.
Indemnity Health Insurance Plans
Indemnity health insurance is a unique type of plan that lets you select the healthcare provider of your choice, be it a primary care physician or hospital. Another term used for this type of insurance is fee-for-service plan. An indemnity health insurance policy is unique from an HMO or PPO plan because it allows you to choose where you want to receive care. You can even self-refer when making an appointment with a specialist.
Health Reimbursement Arrangements (HRAs)
A Health Reimbursement Arrangement (HRA) lets employers fund their employee’s health coverage in a streamlined fashion. No expensive health plan is needed. The employer sets up the plan, which reimburses employees for medical expenses. Any unused balances can be carried forward.
Spouses and dependent children up to age 27 may also be included in an HRA, and both the employer and the employee can get tax benefits from this deal. The Internal Revenue Service provides specific regulations on how such plans can be set up. So, for example, if your child needs an x-ray, you can ask your employer to reimburse the amount you paid.
High-Deductible Health Plan
A high-deductible health plan, HDHP, offers the user lower monthly premiums in exchange for a higher deductible. In 2020, a plan qualifies as an HDHP if the deductible is at least $1,400 (for individuals — for a family, that number jumps to $2,800 or more).
This can save money on a month-by-month basis but you will have to pay more out-of-pocket expenses until you meet your deductible. You might consider combining an employer-sponsored HDHP with a health savings account (HSA) or health reimbursement arrangement (HRA).
Health Savings Account (HSA)
A health savings account, HSA, is similar to a savings account. However, you use it exclusively for medical bills. You deposit money into the HSA — this isn’t taxed. To open an HSA, you have to have a high-deductible plan in place first.
The logic behind this model, which isn’t controlled by the insurance company or your employer, is that people will be smarter about how they invest their healthcare money if they are controlling that money. An HSA is generally best for people who are in good health and thinking primarily of saving for future expenses. If you need expensive medical care now, however, the high deductible demanded of this arrangement can be a hurdle.
Catastrophic Insurance
Catastrophic health insurance is designed to protect you in the event of major medical expenses. They typically come with a lower premium but a higher deductible. Until you reach that deductible, you have to pay the majority of your healthcare expenses out of pocket. This is specifically designed for extreme health care costs, like if you’ve been in a serious car accident. Given that fact, you may reach the deductible quite quickly.
The maximum out-of-pocket cost for catastrophic insurance plans in 2020 is $8,150 under the Affordable Care Act (ACA). Note that you are only eligible for this type of insurance if you are under age 30 or if you qualify for a hardship or affordability exemption.
Which Type of Plan Is Right for You?
There is no one right answer. The right health insurance plan for you depends on everything from your employer to your current health, as well as whether you have any dependents. An insurance company provider can discuss which plan type best suits your needs.